Let’s be honest: most of us don’t think about digestion until something goes wrong. Then suddenly, you’re Googling symptoms at 2 a.m., wondering if that bloated feeling is just last night’s pizza or something more sinister.
Here’s the good news: your digestive system is remarkably responsive to change. Give it the right inputs—water, fiber, movement, less stress—and it often rewards you with smoother operations within days. This guide covers everything from quick wins you can implement before your next meal to the deeper lifestyle shifts that transform gut health for good.
Introduction to Digestive Health
Your digestive system—sometimes called the gastrointestinal (GI) tract—is basically the unsung hero of your body, working 24/7 like that friend who always shows up to help you move but never asks for anything in return. When your gut is crushing it, you don’t even think about it. But when things go sideways? Oh boy, suddenly you’re dealing with stomach pain, bloating, or bathroom irregularity that makes you question every life choice that led you to this moment!
Here’s the thing nobody tells you: a healthy digestive system is absolutely ESSENTIAL for breaking down foods, absorbing all those fancy nutrients you paid extra for at the grocery store, and keeping your immune system from throwing tantrums. Plot twist – a huge chunk of your body’s immune defenses are literally hanging out in your gut right now, standing guard like tiny bouncers protecting you from illness and inflammation. And get this: tons of factors mess with your digestive health, including what you eat, how stressed you are, and whether you actually have any semblance of healthy daily habits. For example, loading up on fiber-rich foods, whole grains, and lean meat can totally support your digestion and help you dodge those not-so-fun digestive diseases like irritable bowel syndrome (IBS), inflammatory bowel disease, and gastroesophageal reflux disease.
But here’s the kicker – poor lifestyle choices or chronic stress can completely wreck your digestion faster than you can say “why does my stomach hate me?” leading to uncomfortable symptoms that make you feel like your body is staging a rebellion, and honestly, increasing your risk for more serious health conditions that nobody wants to deal with. By actually understanding how your digestive system works instead of just hoping for the best, and making small but consistent changes that don’t require a complete life overhaul, you can totally support your overall health and well-being—and it all starts with whatever you decide to put in your mouth at your next meal!
Start Here: Fast Tips to Improve Digestion Today
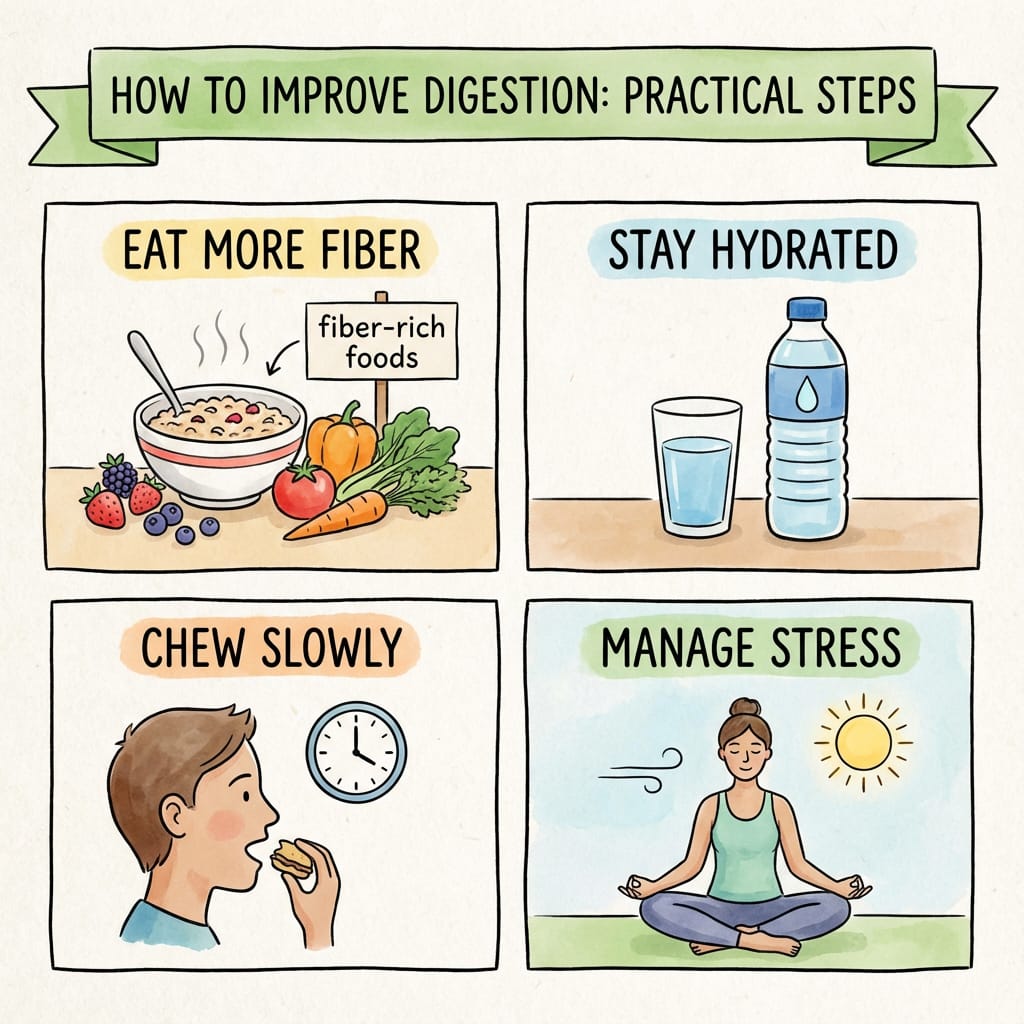
Most people can feel digestive improvements within one to two weeks by changing just a few habits: hydration, fiber, movement, and stress. You don’t need a complete lifestyle overhaul—you need a starting point.
- Drink a glass of water with every meal (breakfast, lunch, and dinner) to keep things moving through your digestive tract.
- Stay hydrated throughout the day, as adequate water intake is essential to prevent constipation and support healthy digestion.
- Start your morning with warm water and added lemon or fennel seeds to help jump-start your colon.
- Add one piece of fruit or a handful of vegetables at lunch and dinner—fruits and vegetables are key sources of fiber and nutrients that support digestive health and overall well-being.
- Aim for a high fiber diet by including whole grains, legumes, fruits, and vegetables to promote regularity and overall gut health.
- Try eating two kiwis per day to improve digestive regularity.
- Walk for 10 minutes after your largest meal to stimulate bowel movements and reduce bloating.
- Eat without screens at least once a day to activate your body’s “rest-and-digest” mode.
- Be mindful of what you eat food and track your intake and symptoms to help identify potential triggers for digestive issues.
- Avoid large meals close to bedtime and wait 2–3 hours before lying down to reduce reflux symptoms.
- Go to bed at a regular time (like 10:30–11:00 p.m.) to support your gut’s natural repair cycle.
- Chew your food slowly and put your fork down between bites.
Food typically takes about 28 to 72 hours to move through the digestive tract, which means changes may reduce bloating and constipation within a few days. If you have existing conditions like irritable bowel syndrome IBS, gastroesophageal reflux disease (GERD) (which causes uncomfortable symptoms like heartburn and indigestion), ulcerative colitis, or Crohn’s disease, work with a gastroenterologist rather than relying on diet changes alone.
Understand Your Digestive System
Your digestive system is essentially a 30-foot processing plant that transforms the sandwich you ate at lunch into the energy that powers your afternoon. The digestive tract—from mouth to colon—breaks food into nutrients your body can actually use. According to U.S. estimates from the 2020s, roughly 60 to 70 million Americans live with digestive diseases, which means you’re far from alone if something feels off.
- Normal transit time ranges from roughly one to three days; when things slow down, you get constipation; speed up, and you’re dealing with diarrhea, bloating, or reflux
- Key organs and their roles: the stomach breaks down protein with acid, the small intestine handles most nutrient absorption with help from the pancreas and liver (which produces bile for fat digestion), and the large intestine absorbs water and houses your gut bacteria
- Digestion connects to whole-body health in ways you might not expect—your immune system (roughly 70% lives in your gut), energy levels, mood through the brain-gut axis, and nutrient status including iron, B12, and vitamin D all depend on a well-functioning digestive system
- The gut microbiome refers to the trillions of microbes living in your colon that help digest fiber, produce vitamins, and interact with your immune system—think of it as an internal ecosystem that influences everything from inflammation to mental well being

Hydration: Water and Hydrating Foods
Low fluid intake is one of the most common—and most overlooked—causes of constipation and sluggish digestion. Before you overhaul your entire diet, make sure you’re actually drinking enough. Water keeps everything soft, slippery, and moving.
- Daily water guidance: around 11.5 cups (2.7 liters) of total fluids for most adult women and 15.5 cups (3.7 liters) for most adult men; about 20% can come from foods, so you don’t need to chug it all from a bottle
- Practical habits: drink a glass of water upon waking, one glass with each meal (breakfast, lunch, dinner), and one between meals; increase intake if you’re sweating, exercising, or in hot weather
- Hydrating foods to add daily: cucumber, watermelon, oranges, strawberries, lettuce, tomatoes, and broth-based soups—aim for at least two to three servings spread throughout the day
- Proper hydration keeps stool soft and easier to pass, reducing straining and the risk of hemorrhoids; if your stool looks like dry pebbles, you probably need more water
- Limit high-sugar sodas and excessive alcohol or caffeine, which can irritate the gut or worsen reflux in some people—plain water remains the evidence-based recommendation for optimal digestive health
Fiber: How Much, Which Types, and How to Add It Safely
Fiber keeps things moving, feeds beneficial gut bacteria, and can lower the risk of diabetes, heart disease, and some digestive problems like diverticular disease. Following a high fiber diet is essential for maintaining digestive health and can also help prevent chronic diseases such as diabetes and heart disease. It’s the single most underconsumed nutrient in the modern diet, and your gut notices.
- Daily targets: about 25 grams of fiber for most adult women and about 38 grams for most adult men; build up gradually over one to two weeks to avoid gas and bloating
- Soluble fiber dissolves in water, helps soften stool, and regulates blood sugar and cholesterol; insoluble fiber adds bulk and speeds transit—you need both for optimal digestion
- Soluble fiber foods: oats, barley, beans and lentils, apples, citrus fruits, carrots, and ground flaxseed; include at least one serving at breakfast and one at dinner
- Insoluble fiber rich foods: whole wheat or whole grain bread and pasta, wheat bran, brown rice, quinoa, nuts, and vegetables like broccoli and green beans—these add the bulk that helps things move
- To increase fiber safely, swap white bread and rice for whole grains versions over seven to ten days; drink plenty of extra water as you add more fiber to prevent the exact constipation you’re trying to fix
- People with active inflammatory bowel disease flares or strictures should follow medical advice before dramatically increasing fiber intake

Build a Gut-Friendly Plate: Fats, Protein, and Cooking Methods
What you eat with your fiber—fats, proteins, and how foods are cooked—can either calm or irritate the digestive system. The goal isn’t perfection; it’s building a plate that works with your gut instead of against it.
- Choose lean meat and proteins for easier digestion: skinless chicken or turkey, fish like salmon or cod, eggs, tofu, and legumes; limit fatty cuts of beef, red meat, pork, and processed meats like bacon and sausages to a few times per week at most, as these foods often contain increased levels of chemicals and additives, which may pose health risks
- Healthy fats (olive oil, avocado, nuts, seeds, omega-3-rich fish) support digestion by stimulating bile production for fat breakdown and enabling absorption of fat-soluble vitamins A, D, E, and K; use small portions like one to two tablespoons of olive oil or a small handful of nuts per meal
- Very greasy, fried foods can slow stomach emptying and worsen heartburn or indigestion, especially at night—save the deep-fried indulgences for occasional treats rather than daily habits
- Gentler cooking methods support better digestion: steaming vegetables, baking or grilling fish and poultry, poaching eggs, and boiling or pressure-cooking beans and lentils make foods easier to break down
- Sample gut-friendly day: oatmeal with berries and nuts for breakfast, a quinoa and vegetable salad with grilled chicken for lunch, and baked fish with brown rice and roasted vegetables for dinner—whole foods prepared simply
Support Your Microbiome with Probiotics and Prebiotics
Probiotics are beneficial live bacteria; prebiotics are the fibers that feed those bacteria. Both influence digestion, immunity, and even mood through the gut-brain connection. A healthy microbiome isn’t just about taking probiotics—it’s about creating an environment where good bacteria can thrive.
- Common probiotic foods: live-culture yogurt, kefir, kimchi, sauerkraut, miso, tempeh, and fermented pickles; adding one to two small servings per day introduces friendly bacteria that support digestion
- Probiotics can be particularly useful after a course of antibiotics or for some people with IBS symptoms or antibiotic-related diarrhea, though evidence remains strain-specific and still evolving
- Prebiotic fibers and where to find them: onions, garlic, leeks, asparagus, bananas (especially slightly green), oats, barley, and chicory root; include a variety across the week to maintain a diverse microbiome
- People with sensitive guts or IBS may react to some high-FODMAP prebiotic foods—working with a dietitian before major changes prevents unnecessary digestive symptoms
- Avoid self-prescribing high-dose probiotic supplements without medical input, especially if immunocompromised; food sources of probiotics offer other benefits beyond just the bacteria themselves, including essential nutrients and fiber
- Some dairy products like yogurt and kefir serve double duty as both protein sources and probiotic foods, making them efficient choices for gut health
Lifestyle Habits: Movement, Routine, and Stress Management
Daily habits—movement, sleep, stress, and timing of meals—strongly affect digestion through the brain-gut connection. Your nervous system directly controls digestive function, which means what happens in your head shows up in your gut.
- Exercise regularly with at least 150 minutes per week of moderate physical activity like brisk walking or cycling; even 10 to 15 minute walks after meals can stimulate bowel movements and reduce bloating
- Chronic stress triggers or worsens IBS, reflux, and functional bowel disorders by shifting your nervous system away from “rest-and-digest” mode; exam periods, work deadlines, and caregiving stress all take a toll on your gut. It’s essential to manage stress to support gut health and improve digestion.
- Simple stress-management tools to start immediately: five-minute deep-breathing routines, short guided meditations, yoga, journaling, or spending time outdoors daily—these help reduce stress and promote parasympathetic nervous system dominance
- Establish regular meal times (breakfast between 7–9 a.m., lunch between 12–2 p.m., dinner before 8 p.m.) and avoid skipping meals or heavy late-night eating, which conflicts with your body’s natural rhythms
- Aim for seven to nine hours of consistent sleep each night; irregular or short sleep worsens inflammation, reflux, and food cravings that harm digestion and overall health
- Reducing or quitting smoking and limiting alcohol and high caffeine intake can dramatically improve reflux, ulcers, and diarrhea symptoms—these lifestyle changes often matter as much as dietary ones

Eating Behaviors: How You Eat Matters
Digestion begins in the mouth, and speed, posture, and attention while you eat can change symptoms like gas, bloating, and heartburn. The mechanical act of eating—not just what you eat—directly influences how well your body processes each meal.
- Chew thoroughly, aiming for slower bites and putting utensils down between bites; this allows salivary enzymes to begin breaking down food and reduces large, hard-to-digest pieces reaching your stomach
- Practice mindful eating: avoid screens during at least one meal per day, focus on flavors and fullness cues, and take 15 to 20 minutes to complete a meal instead of rushing—research shows this approach reduces stress and supports digestive function
- Maintain upright posture during and for at least 30 to 60 minutes after eating to reduce reflux, especially important for those with gastroesophageal reflux disease
- If you experience frequent heartburn, avoid lying down within two to three hours of large meals and consider smaller, more frequent meals if recommended by your doctor
- Try keeping a food and symptom journal for one to two weeks, noting what was eaten, time, and symptoms (bloating, stomach pain, stool changes) to spot personal triggers like certain dairy products, gluten-containing foods, very spicy dishes, or artificial sweeteners
- Avoid aggressive elimination diets without professional guidance from medical professionals, as they can lead to nutrient deficiencies and unnecessary restrictions that harm rather than help
Foods to Avoid
While a balanced diet is absolutely crucial for keeping your digestive system happy, certain foods are basically declaring war on your gut—especially if you’re one of those unlucky souls dealing with irritable bowel syndrome or other digestive drama! Fried foods? Oh boy, these greasy troublemakers are like sending your stomach on a roller coaster it definitely didn’t buy a ticket for. They’re notorious for turning your digestive system into a confused, sluggish mess because your poor gut is sitting there like “HOW am I supposed to break this stuff down?!” These foods basically hit the brakes on your stomach emptying and unleash a parade of uncomfortable symptoms that’ll have you questioning every life choice, especially if you go wild with portions or decide to wage this battle right before bedtime.
High-fiber foods are usually the heroes of the digestive world, but here’s the plot twist—for some people, especially those dealing with IBS, dumping too much fiber into your system at once is like throwing a fiber party your gut wasn’t ready to host! Instead of smooth sailing, you get gas, bloating, and stomach pain that makes you feel like your digestive system is staging a full revolt. If you’re experiencing this fiber rebellion, it might be time to slow your roll and introduce these fibrous friends gradually instead of going from zero to fiber superstar overnight.
And then we have dairy products—the sneaky culprits that can turn your gut into a battlefield! For anyone dealing with lactose intolerance or sensitivity, milk, cheese, and ice cream might as well come with a warning label that says “PREPARE FOR DIGESTIVE CHAOS.” These seemingly innocent foods can unleash a symphony of bloating, gas, and other gut disasters that’ll have you wondering why you thought that extra slice of pizza was a good idea. If you suspect your beloved dairy is the villain in your digestive story, try giving these foods the boot temporarily and see if your gut throws you a thank-you party!
The secret sauce? Pay attention to how your body reacts to different foods like you’re a detective solving the case of your cranky digestive system! By making mindful choices and actually listening to what your gut is trying to tell you, you can kick those uncomfortable symptoms to the curb and finally give your digestive system the love and support it’s been desperately asking for.
Common Digestive Issues
Are you tired of dealing with stomach troubles that seem to pop up at the worst possible moments? Trust me, you’re NOT alone! Digestive issues are ridiculously common and can range from those “oh no, not now” mild moments to serious chronic conditions that basically hijack your entire day. The three troublemakers you hear about most? Irritable bowel syndrome (IBS), inflammatory bowel disease (IBD), and gastroesophageal reflux disease (GERD) – and boy, do they know how to make their presence known!
So what’s the deal with these digestive drama queens? Irritable bowel syndrome IBS shows up with abdominal pain that feels like your gut is throwing a tantrum, bloating that makes you look six months pregnant, and bowel habits so unpredictable they could win an award for chaos. Then there’s inflammatory bowel disease – the overachiever of the bunch that includes Crohn’s disease and ulcerative colitis. This one brings chronic inflammation to your digestive tract like an unwelcome house guest, serving up persistent stomach pain, diarrhea, and fatigue that makes you feel like you’ve been hit by a truck. And don’t even get me started on gastroesophageal reflux disease! This troublemaker delivers heartburn that feels like a fire-breathing dragon took up residence in your chest, regurgitation episodes, and burping sessions that make eating and sleeping about as comfortable as sleeping on a bed of rocks.
Here’s the thing – these conditions can absolutely wreck your overall health and turn your well-being upside down! If you’re experiencing ongoing digestive drama or notice your usual patterns have gone completely rogue, it’s time to wave that white flag and consult a healthcare provider. Seriously, don’t tough it out! Early diagnosis and proper management are your secret weapons to taking back control and getting your quality of life back on track where it belongs.
Additional Tips
Beyond stuffing your face and sweating it out at the gym, there are some other tricks that’ll keep your gut from staging a daily revolt against you. Here’s the thing nobody wants to admit: stress literally makes your intestines freeze up like a deer in headlights. So yeah, when you’re freaking out about deadlines, your digestive system basically goes “nope, we’re closed for business.” That’s why meditation, deep breathing, or some gentle yoga actually works – it’s like telling your gut “hey, it’s safe to do your job now.” And get this: good sleep and keeping your weight in check aren’t just for looking good in photos. They’re basically the difference between your digestion running like a well-oiled machine versus sputtering along like a broken-down car.
Your lifestyle choices? They matter more than you think, and some of them are probably sabotaging you right now. Smoking is basically like setting tiny fires in your digestive tract (sexy, right?), and while that glass of wine feels relaxing, too much booze turns your gut into a grumpy, inflamed mess. Cut back on these gut destroyers and you’ll actually lower your chances of developing the kind of serious digestive problems that nobody wants to Google at 2 AM.
Now here’s where it gets interesting: probiotic supplements and foods like yogurt and kefir are basically like hiring a cleanup crew for your intestines. These little bacterial helpers maintain the microscopic ecosystem that keeps everything moving smoothly and prevents your gut from turning into a war zone. It’s the kind of boring maintenance work that pays off big time when you’re not doubled over wondering why your stomach hates you.
Combine all this stuff with eating actual food instead of whatever passes for nutrition these days, and you’ll have a digestive system that works with you instead of against you. Your gut will thank you, and more importantly, you’ll stop having those awkward conversations with your bathroom mirror.
When to See a Doctor About Digestion Problems
While everyday bloating or mild constipation often improves with lifestyle changes, some digestive symptoms require prompt medical attention. Knowing the difference between “annoying but manageable” and “needs professional evaluation” can protect your health and give you peace of mind.
- Red-flag symptoms requiring medical evaluation: unintentional weight loss, blood in stool (bright red or black, tarry stools), persistent vomiting, severe abdominal pain, difficulty swallowing, or new nighttime symptoms that wake you up—these could indicate serious health conditions
- Common digestive conditions like gastroesophageal reflux disease, irritable bowel syndrome, celiac disease, ulcerative colitis, Crohn’s disease (inflammatory bowel disease), and colon cancer can only be accurately diagnosed by a healthcare provider through proper testing
- Age-based screening matters: in many places, routine colorectal cancer screening now starts around age 45 for average-risk adults, earlier if there’s a strong family history or other risk factors—this screening has many health benefits and catches problems early
- Bring a food and symptom diary, medication list, and family history details to your gastroenterology appointment for more targeted care; the more information you provide, the faster they can identify digestive issues
- Combining medical advice with the lifestyle strategies in this article—fiber, hydration, exercise, stress management—can significantly improve digestive comfort and long-term gut health; these approaches work together, not in competition
Your gut isn’t asking for perfection. It’s asking for consistency: enough water, enough fiber, enough movement, less stress, and the occasional check-in with a professional when things feel off. Start with one change today—just one—and build from there. Small shifts, repeated daily, become the foundation of good health that extends far beyond your digestive tract.
Conclusion and Final Thoughts
Look, taking care of your gut is basically the most no-brainer way to stop feeling like garbage and actually prevent your digestive system from staging a full rebellion against you. You know what I’m talking about – loading up on fiber-rich foods, whole grains, and lean meat while actually moving your body and not letting stress turn your insides into a twisted pretzel. It’s like giving your digestive system a roadmap instead of leaving it to figure things out on its own like some kind of intestinal treasure hunt.
Being smart about what foods make your stomach throw tantrums, and actually doing the healthy stuff consistently, is basically you taking the wheel instead of letting your gut drive you around like a cranky toddler. And hey, if you’re sitting there confused or your body keeps sending you weird signals that persist, just call the pros – they’ve seen it all and won’t judge you for that time you ate nothing but pizza for a week.
Here’s the thing nobody really talks about – prioritizing your digestive health isn’t just about avoiding those “why did I eat that” moments. It’s about unlocking the kind of energy that makes you feel like you could tackle anything, dodging those nasty chronic diseases, and actually enjoying your life instead of constantly negotiating with your stomach. Those tiny changes you make every day? They add up to feeling absolutely amazing from your core outward, and trust me, your whole body will thank you for it.